Downton Manor fans won’t readily forget the episode in which Lady Sybil gives birth to her daughter.
You may recall how delirious she became following the delivery of her baby. The doctor diagnosed pregnancy-induced hypertension now commonly referred to as pre-eclampsia, or as the medical profession refer to it as eclampsia exhibiting delirium, visual disturbances, and critically high blood pressure.
In the aftermath of that scene, I reflected poignantly on the memories of my first born baby boy.
In 1999 when I had my first baby, I experienced severe pre-eclampsia which was eventually diagnosed in week 27 of my pregnancy but I suspected that the symptoms had already started as early as week 19.
In April of 1999 and on Dr’s advice my husband and I took a short trip to Hamburg to see friends and family.
When we arrived at the hotel early afternoon I had begun to notice very swollen legs and ankles, they were spongy to the touch, I had a slight headache but nothing else and after packing lay down for a couple of hours. The swelling dissipated and I put it down to a combination of flying and too long on my feet.

We were due to meet the rest of the family in Hamburg the following day.
It was a lovely spring morning and as my husband’s family were so keen for us to see as much of the city as we could we did lots of walking, visited shops and all the usual things a tourist would do when visiting a big city.
Everything was in walking distance and being pregnant and completely unaware of the symptoms of pre-eclampsia again I experienced swelling in my legs and body.
I wasn’t feeling great, my heart was pumping hard and I was angry for trying to push myself.
My husband and his family were taking a trip on a ferry around the river Alster which would be a tour lasting about an hour and a half.
I sat out the trip at a cafe overlooking the river with a cup of tea and a book to read my feet were raised and I had a good view of the people walking by.
And this is how it went on.
At my next antenatal check-up, none of the symptoms were visible.
I suspect the reason was that the waiting time to be seen was always a good hour and my body had the time to rest and my heart rate and blood pressure went back to almost normal and although my blood pressure was slightly elevated this is quite common at the stage of pregnancy I was at.
I was nearing the end of my first year at De Montfort University studying for a postgraduate business degree I was at the final hurdle and we had completed our last group assignment and presentation.
The group who had now become firm friends and I were due to celebrate the completion of our first year in a pub near the college.
I really wasn’t feeling too good and so I had to decline despite nice protestations. Ironically one of my friends said, the hospital is only around the corner so you don’t need to worry.
All I wanted to do was to drive home, lie down and sleep.
As the afternoon wore on I wasn’t getting any better and my husband called me surprised to find me at home. Then a strange conversation took place and I happened to mention to him that I hadn’t pee’d since the morning and had no desire to pee and I had had a mild but persistent headache.
As I was at week 33 I figured it was the usual condition of a heavily pregnant woman but I called the midwife out to see me that afternoon to be sure.
When she took my blood pressure she visibly paled in front of me, she asked me to move on to my right side to take the pressure off my heart and then she checked my very spongy ankles and legs and was clearly worried.
She asked me how long I had been like this, since week 19-20 I said.
Calmly she explained that I had pre-eclampsia and that I would need to go to the hospital immediately.
As luck would have it my husband walked through the front door so there was no need for the ambulance thank god. I quickly packed a bag and I was advised that someone would meet us at the maternity unit. I was admitted into Hospital all the checks were done and every-time I needed the toilet I had to pee into a container for measuring purposes to see how much output my body was creating.
Finally, after 24 hours of no sleep and sharing a ward with 3 lovely women and one woman who snored so loudly and kept us all awake, I beckoned the registrar and insisted that I should be allowed to go home. There was no way I was staying in the hospital for 4 weeks coupled with the fact I had a business to run as well.
He finally agreed to release me, on the proviso that I had to sign some medical forms (non-disclaimer) and that I had to come to the maternity unit every morning for a full checkup. I agreed to this as I felt that if I was in my own home I would be calmer and relaxed than I would be if I was in the hospital.
I was prescribed labetalol high blood pressure tablets to keep the blood pressure down and my urine was tested every day but nothing changed.
Despite me trying to manage the condition by telling myself to keep calm, resting on the sofa and sleeping my condition worsened and by 37 weeks of pregnancy my condition was so severe that I finally had to be admitted into the maternity unit.
June 12th, 1999 was the evening the consultant and theatre nurses were fearful that I would go into an eclamptic shock.
My husband described me as a baby elephant with skin so flushed and spongy (oedema the body retains fluid) due to protein in the urine (proteinuria) and the kidneys unable to process it.
My blood pressure was so high that my consultant explained that unless I was admitted into surgery NOW for a Caesarean section then in all likelihood the life of my unborn child and myself would be in serious jeopardy.
It was a traumatic time more for my husband and baby because I had reached that point of dis-association, aware of what was going on but unable to process my thoughts clearly and meaningfully. I recall the headache and visual disturbances, sickness and feeling so ill that I simply couldn’t process that my body had reached the point where a natural delivery was impossible.
I do recollect my insistence on having a local rather than a general anaesthetic. I am very determined and was emphatic about wanting to be awake during the procedure. The surgeon was doubtful but something somewhere was urging me to remain awake even if it meant in a half-lucid state.
By remaining awake during the operation I felt that at least I could focus on what was happening and maybe manage and control my body.
Following the birth of our beautiful baby boy, I spent the next 36 hours in intensive care, 22 litres of fluid came out of my body via the catheter. I was in a semi-comatose state unable to speak clearly but aware of what was going on around me. My blood pressure was still critically high and my husband was advised that although our baby had been delivered there was a high probability I could go into an eclamptic shock.
I eventually came out of the danger zone and 4 days later developed a post-op infection that bought on a high fever which meant my stay in hospital amounted to 10 days.
When I finally arrive home with our new bundle of joy it felt such a relief.
I continued with high blood pressure tablets for some weeks later following the birth and was monitored by the Dr and midwife but I was left anaemic and tired. Suffice to say I lived to tell the tale. My patients are sometimes interested what is the worst thing that can happen to them with Levitra 20mg. Very uncommon adverse reactions affecting up to one person in 1500 include swelling of the mucous membranes and skin, as well as your throat, lips and face (allergic reaction); sleep disturbances, drowsiness, stuffy nose, impaired touch or numbness, dizziness, ringing in the ears, shortness of breath, dry mouth, nausea, palpitations or increased heart rate. As a rule, these are easy to manage, after which you’ll need to visit your doctor’s office and get another medication prescribed.
In 2003 I had a second baby boy and again I experienced pre-eclampsia. This time my husband and I knew what to expect and I was better prepared both mentally and emotionally for what was to come.
My midwife, Dr and consultant were on hand to monitor and manage the pregnancy. It was nowhere near as traumatic as the first but I required an emergency Caesarean section to deliver him.
In fact, giving birth to my second boy, Michael turned out to be easier and I am certain this was because I had more knowledge, I was more relaxed and I am sure this made the management of the condition easier.
What is pre-eclampsia?
In 1999, research and information about pre-eclampsia were thin on the ground, sketchy at best and it was difficult to find any information about the condition.
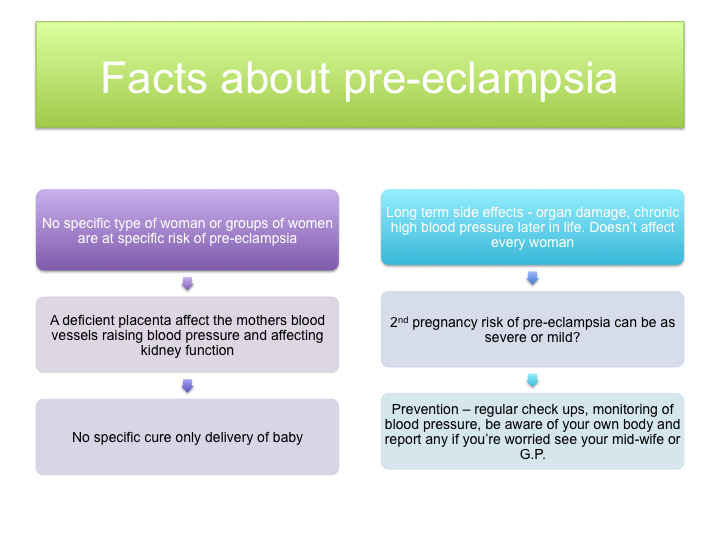
Pre-eclampsia or preeclampsia is a medical condition characterised by high blood pressure and significant amounts of protein found in the urine of a pregnant woman. If left untreated, it can develop into eclampsia, the life-threatening occurrence of seizures during pregnancy.
Mild pre-eclampsia affects approximately 1 in 10 of all pregnancies making it the most common serious complication of pregnancy.
There are no specific determining factors that have been singled out as to the cause of pre-eclampsia but the placenta in pre-eclamptic pregnancies becomes defective.
The placenta supplies oxygen and nutrients to the baby via the mothers’ blood.
Pre-eclampsia may develop from 20 weeks’ gestation (it is considered early before 32 weeks) with the majority of cases occurring in the final trimester.
The nature of pre-eclampsia makes it the ‘silent killer’ because in its earliest stages it is symptomless. Regular antenatal care is a prerequisite because the standard antenatal checks include monitoring of blood pressure and urine testing for protein (proteinuria) will raise a trigger that a mother requires additional antenatal monitoring.
Pre-eclampsia is characterised as a ‘multi-system disorder’ because it affects different parts of the body – liver, kidneys, cardio-vascular and clotting systems.
Mild pre-eclampsia affects up to 10 per cent of first-time pregnancies with severe pre-eclampsia affecting 1-2 of every 100 pregnancies.
Every year in the UK, 1,000 babies die as a result of the effects of pre-eclampsia largely as a consequence of premature delivery and 7 mothers die each year from the severity of the condition.
What are the causes and symptoms of pre-eclampsia?
There is no specific set of factors that make a woman more susceptible to pre-eclampsia although there is a train of thought that suggests first time pregnancies, older women (over 35’s) younger mothers (under 2o) carrying twins, women with diabetes, high blood pressure, kidney disease, women with a short stature and women with a BMI (body mass index) of more than 30.
Genetic factors may play a part since women whose mothers had pre-eclampsia may be pre-disposed to the condition. The condition originates in the placenta which links the mother to the baby.
The placenta needs a large supply of blood from the mother to sustain the growing baby and with pre-eclampsia the placenta can’t provide enough blood because the demands placed upon it are very high as is the case with carrying twins or simply that the arteries in the womb didn’t develop as they should have done when the placenta was being formed.
How is pre-eclampsia detected?
In the early stages, pre-eclampsia can be symptomless and can only be detected with routine antenatal tests. If blood pressure is monitored and there is a noticeable rise coupled with the protein in the urine and body swelling of the face, hands, feet caused by fluid retention indicates it is likely to be pre-eclampsia.
Blood pressure rises in the pregnant mother which affects the kidney function and waste products instead of being excreted in the urine accumulate in the blood and blood proteins leak into the urine. The mothers liver, lungs brain and clotting system can also be affected.
In the final stage of the condition – eclampsia, convulsions, stroke, pulmonary oedema (fluid in the lungs), kidney failure, liver damage and breakdown of the blood clotting system are the most dangerous complications.
There is no single diagnostic test to detect the early signs of pregnancy. Although recent research by the American Society of Nephrology is developing a test that can detect specific kidney cells in patients’ urine more work is required to enable it to be an accurate and positive test for pre-eclampsia.
A dietary supplement in the form of amino acid and antioxidant vitamins have also been tested on a group of 600 women in Mexico City, some with given a placebo and the remainder were given food bars containing L-arginine and antioxidant vitamins.
In the placebo group, it was found 30.2 per cent of women developed pre-eclampsia and 12.7 per cent in the group given the L-arginine and antioxidant vitamins. (Source: BBC News Health 2011)
The above studies are inconclusive and more research and studies are required into the condition.
Given all of the above, most women understandably might be fearful to go on and have another baby. Having experienced severe pre-eclampsia didn’t deter me but what helped was understanding the condition and being more aware of the symptoms which were acquired through my own research and talking to the consultants who attended to me.
Frustratingly it is not a condition that can be controlled, managed yes, by good antenatal checks. The condition is only ‘cured’ by delivery of the baby the challenge is ensuring mother and child can safely get to 37 weeks reducing the possibility of delivering a premature baby.
For more information on pre-eclampsia, you can visit APEC – Action on Pre-Eclampsia. An invaluable site providing information about the condition.
Please follow us on Twitter and we need some more likes on our facebook page. You can connect with us on LinkedIn
Have you had pre-eclampsia? How did it affect you? Please share your experience with us on Facebook or drop a comment below.